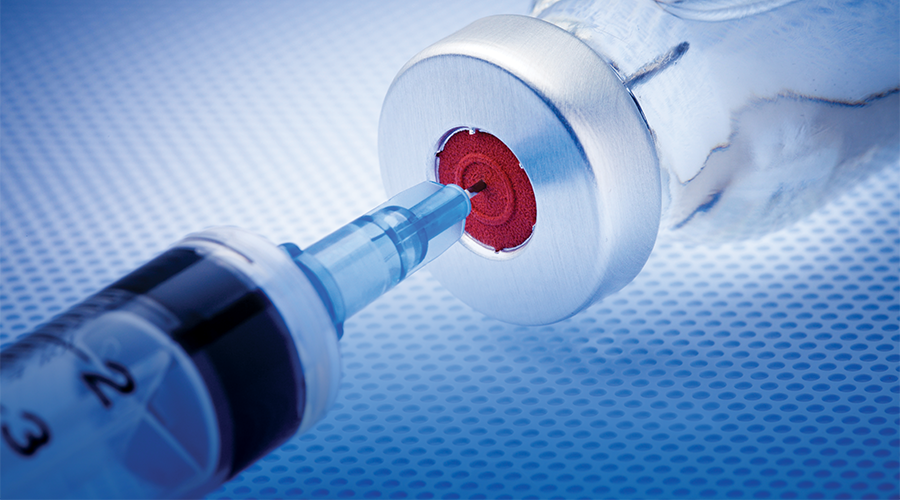
Tis the season. Not the usual season of gifts under the tree, or choral congregations, or festive feasts. Whatever joyful holiday anticipation typically fills the air this time of year is being bagged up by the meanest grinch in the history of Christmas: the coronavirus. As the dangerous virus threatens to prevent celebrations and continues to infect millions of Americans, the greatest gift pharmacists can give their patients this year is immunity. ‘Tis the season of vaccines.
“This is an excellent opportunity for pharmacists to demonstrate their value by stepping up in the face of an unprecedented health crisis. It’s kind of what we do,” said John Beckner, senior director of strategic initiatives at the National Community Pharmacists Association (NCPA). “Our members are able to help the communities that they serve by offering a variety of pharmacy services—and immunizations are one of the most prominent ones. I think it’s a good opportunity to be part of the solution and show others through our actions that we are a valued and essential part of the solution.”
One Covid-19 vaccine, by Pfizer-BioNTech, has already been authorized and begun distribution, while Moderna’s is expected to be authorized this week. About three more US vaccines are in phase 3 trials.
At the same time, with experts warning of a “twindemic,” the demand for the influenza vaccine is at an all-time high. According to Bloomberg, CVS has already given more flu vaccines this year than they did all of last year, and they expect to double the number by the end of the flu season.
On top of that, enough people need to make up vaccinations they delayed during this pandemic that the Department of Health and Human Services (HHS) issued emergency authorization allowing all pharmacists, student interns, and qualified technicians to administer vaccines to children aged 3 to 18. “During Covid we were seeing people less willing to go into their physicians’ offices and other locations, and physicians’ office hours were being modified, so access was harder,” said Mitch Rothholz, chief of governance and state affiliates for the American Pharmacists Association (APhA). “With the order, they declared the reduced childhood vaccination rate as a public health emergency.”
So, ’tis the season. Are pharmacists ready to deliver?
Vaccine distribution plan
The government plans a multi-phased and multi-faceted vaccine distribution process based on supply, storage and handling, and documentation requirements. Although the distribution will be coordinated federally, it will rely heavily on individual states to determine distribution to administration sites in their jurisdiction. Populations most at risk will be prioritized, along with frontline workers, but many details of the distribution depend on which vaccine is approved. The HHS wrote, “Some variables that will impact the planning of this vaccination program are unknown until a vaccine is authorized or approved by the Food and Drug Administration (FDA), such as populations for whom a given vaccine is most appropriate, distribution and storage requirements, dosage requirements, and other variables.” For example, Pfizer, whose vaccine requires storage at negative 94 degrees Fahrenheit, plans to skip the wholesaler and ship directly to sites themselves.
Distribution will occur in three phases, according to the Operation Warp Speed distribution strategy. The first will be the distribution of limited doses with highly targeted administration to achieve coverage in priority populations. The second will be the distribution of large quantities of vaccine to widespread populations—essentially, enough for everyone who wants one. The third will integrate the vaccine into routine vaccination programs, if a vaccine is still needed. It is expected that most independent community pharmacies will get involved in phase two, which could happen within months after the vaccine receives initial approval. Already manufacturers have produced tens of millions to hundreds of millions of their vaccines to be ready to ship as soon as the FDA and CDC give them the go-ahead.
Pharmacy in the spotlight
One thing this distribution plan reveals is the stark change in perception toward pharmacies over the last decade. Back in 2009 when H1N1 vaccines were being distributed, pharmacies were almost an afterthought. “If you look closely, the pharmacy community was not involved at the start of that. It was halfway or toward the end of the process,” Beckner said. “I think the impact that pharmacists had on getting people access to that vaccine was the springboard for gaining authority in the remaining states and for pharmacy- administered vaccinations being more readily accepted by public health and the medical community.”
Almost a quarter of the H1N1 vaccines were administered by pharmacies, and a study from the CDC concluded that pharmacies helped reach 80 percent of the population seven weeks faster than they would have without them during the pandemic.
Now, for the coronavirus pandemic of 2020, HHS has already recognized the importance of pharmacies in the distribution and administration of the vaccine. And in its distribution plan for the Covid-19 vaccine, the CDC explicitly references the H1N1 pandemic as an influence on this plan:
“The Covid-19 pandemic has likely accelerated a trend towards different ways of engaging with the healthcare system, and successful delivery of this vaccine will need to incorporate new types of sites and approaches for vaccine delivery. For example, during H1N1, once vaccines became widely available pharmacies played an important role in the vaccine distribution; pharmacies’ role is even more critical to vaccinations today and will be fully integrated into the distribution plan.”
Already, the government has partnered with CVS and Walgreens to distribute vaccines to long-term care facilities, a key part of reaching the most vulnerable populations first. The CDC also announced partnerships with the national chain pharmacies and independent pharmacy networks—including CPESN, Health Mart, and Medicine Shoppe—to achieve nationwide vaccine distribution.
The distribution timeline for independent community pharmacies will likely depend primarily on the demographics it serves as well as the number of surrounding healthcare facilities and other administration sites. For example, pharmacies in rural areas without other vaccine providers should expect higher prioritization than pharmacies in an urban area next to a health clinic and national chain pharmacy. At some point, every pharmacy will have its turn and should be preparing now.
Covid-19 Vaccine Types
Researchers are testing more than 50 vaccines in clinical trials on humans, and at least 91 preclinical vaccines are under active investigation in animals, according to the New York Times. However, there are only a handful of vaccines in the US with a promising timeline—some perhaps as early as December of this year. To receive FDA approval, a vaccine must demonstrate effectiveness on at least 50 percent of people who get vaccinated.
There are several different types of vaccines being developed. Most of the vaccines work by producing the coronaviruses’s spike protein, which is what enables it to attach to and invade human cells. When the spike protein is produced in the body, the immune system produces antibodies against it, ensuring it will be killed when the real coronavirus enters the system. How they produce that spike protein is what differentiates the various vaccines. Here are the types you need to know.
Genetic
Pfizer-BioNTech, Moderna
New to the vaccine scene, genetic vaccines inject messenger RNA from the coronavirus genome that instructs the body to create its spike protein. These genetic vaccines also induce production of killer T cells, which stop the coronavirus from replicating. This technique relatively new—there are no vaccines of this kind approved for human use. But two of the vaccine frontrunners are using this approach.
Viral Vector
Johnson & Johnson, AstraZeneca
Like genetic vaccines, viral vectors attach a gene (DNA) for the spike protein to a mostly harmless virus (adenovirus), which is injected into the body and carries the gene to its destination and produces the spike protein. The adenovirus is inactive, so it won’t cause any harm.
Protein-Based
Novavax
The spike protein is synthesized in a lab using insects, then injected. This is a typical method for creating vaccines, but they take longer than the other options. They also require an adjuvant booster for the immune system.
Inactivated or Attenuated
Instead of using just the spike protein of the coronavirus, these vaccines inject the entire virus into the body—one that has been inactivated through chemicals or weakened enough to be harmless. The immune system then produces antibodies. This is how the majority of vaccines are made, including the annual influenza vaccine. However, none of the leading US candidates use this technique for the coronavirus.
How should pharmacies prepare?
All vaccinators must meet basic requirements for storage and handling, the details of which we won’t fully know until the vaccine is approved. Some of the frontrunners require refrigeration and will likely require nothing different than routine vaccination storage while others require storage at negative 94 and negative 4 degrees Fahrenheit. Pharmacies do not have to worry about securing or purchasing the vaccines because they will be paid for and supplied by the government. Pharmacies also likely won’t have to worry about ancillary supplies either. According to the distribution strategy, administration sites will be provided with ancillary supply “kits,” which include “needles, syringes, alcohol pads, vaccination cards, and limited PPE.”
One essential requirement is data storage and reporting capabilities. All vaccination information will need to be uploaded to the state immunization information system (IIS) at the very least, and the government may have additional requirements. Among other purposes, the data will serve as a way to know when patients need their second dose and ensure that dose is the same vaccine as their first. According to the HHS, “The vaccination program requires extensive data monitoring infrastructure, including appropriate IT architecture, to incorporate claims and payment processes, to identify when a person needs a potential second dose, to monitor outcomes and adverse events, and to account for products the U.S. government is spending billions of dollars to research, develop, and produce. Data will need to be available both federally and at the state, local, and tribal level to ensure efficient management of the vaccination program.”
Pharmacies hoping to offer the vaccine should get in touch with their state pharmacy association or state health department. Every pharmacy will have to fill out a provider intent form with information about capabilities, such as storage and documentation, and about the demographics of its patients. Rothholz and Beckner said they are trying to coordinate primarily through the state pharmacy associations to reduce the burden on state health departments in having to deal with individual practices.
All pharmacies should be enrolled in VaccineFinder, a service through the CDC that lists you as a vaccine provider and “gives you the opportunity to list all the vaccines you provide,” Beckner said. “That’s another proactive step you can take to get ready for this. They should be doing that anyway if they are an immunization provider.” VaccineFinder will also be used for tracking vaccine supply at practice sites.
Beckner recommends pharmacies get a staffing plan in place to account for the surge in traffic. “I think the demand is going to be unprecedented,” he said. “Pharmacies need to ensure, if they can, to have the appropriate amount of staffing.” Decide on the workflow and format—will you require appointments to control the number of patients in the pharmacy? Will vaccines be administered curbside or at an outdoor station? What personal protective equipment will your staff use? These kinds of decisions should be made long before any vaccine arrives.
The other thing pharmacists need to prepare for, Beckner said, is addressing vaccine hesitancy. “There’s some general mistrust about the vaccine. Is it a political rush to market? Is it safe? I think pharmacists are in a really good position to dispel some of those myths and they need to be prepared to really encourage people to get the vaccine.” Doing that requires an understanding of the vaccine and why it’s safe, which means pharmacists need to do their research. “Education here is going to be huge.”
Is the Covid-19 Vaccine Safe?
One major barrier to broad vaccine uptake is hesitancy from patients who aren’t sure of its safety. Several polls have shown a consistent resistance across the US. In one poll, only 50 percent said they would get a vaccine, 31 percent were unsure, and 20 percent planned not to get it. Side effects were noted as the main reason for the resistance.
Other polls revealed a preference to wait for a while after a vaccine is approved to see if any side effects or adverse events occur.
Pharmacists will have to address vaccine hesitancy, armed with the facts and the ability to demonstrate its safety. In a November media telebriefing Secretary of Health and Human Services Alex Azar outlined the process for vaccine approval, describing five independent checks that work to ensure safety.
1. Clinical trials
“First a vaccine clinical trial has pre-specified end points; they’re statistical and actually these drug companies have been transparent for the first time in history, laying out exactly what those statistical endpoints are. There is a totally independent data and safety monitoring board that will look at the data as it comes in [to] determine if those endpoints have been met. If and only if those endpoints are met that data gets revealed to the company and the FDA.”
2. Manufacturer approval
“The company will have its own second independent process. It will have to meet their ethical standards for submission of an application for either an emergency use authorization or a biologic license.”
3. Review by the Food and Drug Administration
“It’ll come to the FDA, where the FDA will evaluate that vaccine according to two sets of guidances it put out— its general vaccine guidance for Covid and its second EUA guidance for what it would require and expect in terms of approval.”
4. Independent advisory committee
“The advisory committee at the FDA. An external advisory committee that will be webcast. A public external advisory process will advise the FDA.”
5. Approval or authorization by FDA scientists
“All of those elements of the process should reassure the American people that when a vaccine or therapeutic comes out with the authorization or approval of FDA it represents FDA’s career scientists’ best judgment, that it meets their scientific evidence legal and regulatory standards.”
Childhood vaccinations
In addition to the Covid-19 vaccine, pharmacists are being urged to push annual recommended vaccinations, particularly because many Americans missed their doses due to lockdowns and precaution. To increase vaccination access and uptake, the HHS in September authorized pharmacists and student interns to administer vaccines to children aged 3 to 18, later including pharmacy technicians as well. In a press release, the agency wrote, “A May 2020 Centers for Disease Control and Prevention (CDC) report found a troubling drop in routine childhood immunizations as a result of families staying at home. While families followed public health warnings about going out, an unfortunate result was many missed routine vaccinations. This decrease in childhood-vaccination rates is a public health threat and a collateral harm caused by the Covid-19 pandemic.”
This guidance supersedes current state and local laws. About 22 states allow pharmacists to administer pediatric vaccines, which means more than half of the country can’t. Although this is a temporary allowance through emergency authorization, Beckner and Rothholz are hopeful it will open the door for permanent change in those states that currently restrict it. “The HHS provides a window of opportunity to show that we can have an impact. Clearly, from the public health perspective, it will provide additional access and will allow for more people to be protected.” Beckner said. “I think it’s going to be easier for the states to adopt regulations that make this permanent, and some states have already started working on it.”
“The HHS provides a window of opportunity to show that we can have an impact. Clearly, from the public health perspective, it will provide additional access and will allow for more people to be protected.”
The amendment could also facilitate increased dialogue with pediatric providers on this and other issues. “One thing that it does is hopefully allow for more collaboration and acceptance by the pediatric community who have historically been resistant to pharmacists immunizing children,” Beckner said. “If pharmacists can play a role in children and adolescents getting caught up on their regular immunizations, I think the pediatric medical community will be more accepting.” Beckner advises pharmacies to get in touch with the local pediatric providers before they start administering the immunizations, as that could lessen the risk of it becoming a turf issue.
The HHS authorization comes with several requirements, most of which are already met by pharmacists who administer vaccines to adults. One of the requirements is a two-hour ACPE-approved continuing education course on immunizations during each license renewal cycle during the declared emergency. To help pharmacists meet this requirement, APhA, in partnership with Washington State University College of Pharmacy and Pharmaceutical Sciences, has created a new program covering the specifics of vaccinating children aged 3 to 18, which Rothholz referred to as a “refresher course” for pharmacists who have already been through APhA’s immunizing pharmacist certificate training program. This program is an additional offering within APhA’s extensive portfolio of immunization-related educational programs that help pharmacists meet the education requirements of the HHS authorization, Rothholz said.
The expanded authority also requires immunizing pharmacists to educate the patient or their adult caregiver regarding the importance of well-child visits, given that there is a percentage of the population that does not have an existing medical home, Rothholz explained.
The next thing to do is view the pediatric vaccine schedule, which you can find on the CDC’s website, and decide on which vaccines to offer and understand the ages and recommended dosing schedule for each vaccine. Rothholz said, “The authority is from ages three to eighteen. It doesn’t say you have to do three if you aren’t comfortable. We don’t want any practitioner doing anything they aren’t comfortable doing.”
Beckner also recommends becoming involved in the Vaccines for Children program, a federally funded program that provides vaccines at no cost to children who might not otherwise be vaccinated because of inability to pay. “Not a lot of pharmacies are involved in that program because of the administrative burden and reimbursement not being great, but that may be an opportunity in a rural area to really help the community they serve.”
Essential providers
At the end of the day, the pandemic serves as a magnifying glass on the essential role of community pharmacies in caring for the health of our nation, and the Covid-19 vaccine administration is a natural outflow of that reality.
“Community pharmacists have been on the front lines since the Covid crisis began in early March. They want and really should be part of the solution to the crisis,” Beckner said. “They have been the safety net for the communities they serve. They have remained open, for the most part, throughout the crisis while other providers have been forced to close their doors, at least temporarily. They are ready and willing to administer the vaccine once it becomes available to them.”
CDC Guidance Highlights
Although life has resumed in many ways, including the reopening of pharmacy front ends, the coronavirus is still in full swing. The Centers for Disease Control and Prevention has issued interim guidance for routine and influenza immunization services “to assist healthcare personnel in a variety of clinical and alternative settings for the safe administration of vaccines during the Covid-19 pandemic.” Visit the CDC website for the full guidance.
- Require appointments for vaccinations.
- Limit the number of people in the building at any given time.
- Screen for symptoms of Covid-19 before arrival and upon arrival.
- Require face masks for staff and patients over the age of two years (if tolerated).
- Reduce crowding in waiting areas by asking patients to remain outside until they are texted or called in for their appointment.
- Create a separate vaccination area or separate hours for patients at increased risk for severe illness from Covid-19, such as older adults and those with underlying medical conditions.
- Ensure that physical distancing measures are maintained during the entire visit.
- Use electronic communications as much as possible to minimize time in the pharmacy and the reuse of materials (e.g., clipboards, pens).
- Administer all needed vaccines on a single visit, unless a specific contraindication exists, to reduce the number of visits.
From the Magazine
This article was published in our quarterly print magazine, which covers relevant topics in greater depth featuring leading experts in the industry. Subscribe to receive the quarterly print issue in your mailbox. All registered independent pharmacies in the U.S. are eligible to receive a free subscription.
Read more articles from the December 2020 issue:
- Covid-19 and childhood vaccines: everything independent pharmacies need to know
- These are the most common Covid-19 fraud schemes targeting small business
- How Covid-19 relief will affect this year’s taxes for pharmacies
- How to bring in big revenue with a gifts and cards section
- Proven tips to resolve prior authorizations quickly and easily
- This pharmacy saves thousands on its cost of goods
- Why debt can be a valuable financial tool for independent pharmacies
- How to prevent the most common and most expensive pharmacy lawsuits
An Independently Owned Organization Serving Independent Pharmacies
PBA Health is dedicated to helping independent pharmacies reach their full potential on the buy side of their business. The member-owned company serves independent pharmacies with group purchasing services, expert contract negotiations, proprietary purchasing tools, distribution services, and more.
An HDA member, PBA Health operates its own NABP-accredited (formerly VAWD) warehouse with more than 6,000 SKUs, including brands, generics, narcotics CII-CV, cold-storage products, and over-the-counter (OTC) products.
Want more pharmacy business tips and advice? Sign up for our e-newsletter.